09 Jan 2017 – The Year of AI

 Joe Roushar – January 2017
Joe Roushar – January 2017
Intelligent but Artificial
Recently, January 5th, 2017, on my ride into work I was listening to BBC World Update with Dan Damon, as I often do, and heard him interviewing someone about the new artificial intelligence (AI) app for the British National Health Service from Babylon Health (similar story on TechCrunch). It’s a Chat Bot for SMS text messaging that will help people with symptoms of illness enter the trouble they’re experiencing and get recommendations on what to do. The app sounds like a natural evolution in our technical capabilities, yet the BBC couldn’t resist the urge to raise the spectre of machines supplanting humans with a clip from 2001, a Space Odyssey. I have referenced the same myself (1) (2) (3), but not to invoke fear, for heaven’s sake.
Dan had to ask about the risks (I know, that’s his job), and the interviewee pointed out that in Britain, about 1 in 8 diagnoses by human medical professionals are incorrect. In many countries, correct diagnoses are less common. According to the interviewee, the Babylon Health Chat Bot system outperforms that by a healthy margin. I must observe, that this should not be surprising to folks, and anyone who thinks one human doctor or nurse can store as much medical knowledge, juggle as many variables, and diagnose illness as accurately as a well-designed automated system is naïve. Systems cannot yet sense unspoken things, and will not replace sensitive care givers anytime soon, but they already augment medical care in amazing and positive ways.
| Understanding Context Cross-Reference |
|---|
| Click on these Links to other posts and glossary/bibliography references |
|
|
|
| Prior Post | Next Post |
| Curating Digital Meaning | Cognitive Multi-Processing |
Let’s consider automation in healthcare and it’s impact.
Exhibit 1: Charting
 Charting programs have mostly replaced the clipboard in US medicine, and in hospitals and clinics throughout the world. The improvement in outcomes and reduction of errors due to miscommunication have been tremendous. It’s not that doctors and nurses can’t read or write: it’s that digital records are much more readable and clearer. Furthermore, computers provide better templates than paper and can prompt a medical professional to complete critical data and ensure that the data is applied to the correct patient. Add to this, automatic prompting for compliant electronic health and medical records (EHR/EMR) and you have records that are much quicker and easier to retrieve, even from great distances.
Charting programs have mostly replaced the clipboard in US medicine, and in hospitals and clinics throughout the world. The improvement in outcomes and reduction of errors due to miscommunication have been tremendous. It’s not that doctors and nurses can’t read or write: it’s that digital records are much more readable and clearer. Furthermore, computers provide better templates than paper and can prompt a medical professional to complete critical data and ensure that the data is applied to the correct patient. Add to this, automatic prompting for compliant electronic health and medical records (EHR/EMR) and you have records that are much quicker and easier to retrieve, even from great distances.
Exhibit 2: Multi-Layered Imaging
 It takes computers to be able to reassemble dozens or hundreds of layers of images into accurate views in depth. MRIs, CT scans and other significant advances in medical imaging provide minimally invasive perspectives to professionals able to interpret the pictures. Without computers, these technologies would not be possible. Add to this, the ability to tag the image information with metadata, such as the subject’s demographics and other contextual information, and de-identify the name of the subject person, and you have invaluable research tools that do not compromise anyone’s privacy. Once again, computers have contributed to more positive health outcomes by delivering useful information where and when it is needed.
It takes computers to be able to reassemble dozens or hundreds of layers of images into accurate views in depth. MRIs, CT scans and other significant advances in medical imaging provide minimally invasive perspectives to professionals able to interpret the pictures. Without computers, these technologies would not be possible. Add to this, the ability to tag the image information with metadata, such as the subject’s demographics and other contextual information, and de-identify the name of the subject person, and you have invaluable research tools that do not compromise anyone’s privacy. Once again, computers have contributed to more positive health outcomes by delivering useful information where and when it is needed.
Exhibit 3: Automated Risk Reporting
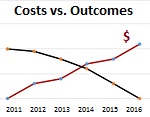 Risk reporting mandates in the US Affordable Care Act created new categories of automated processes and reports under the rubric of “Risk Adjustment, Reinsurance, and Risk Corridors” (3Rs) with the intent of offsetting the impact of rules that protect patients by prohibiting insurers from charging higher premiums or refusing coverage based on preexisting conditions. The motivation was well-intended, but the impact (law of unintended consequences) was opposite of the underlying intent. It cost insurers tens of billions of dollars to implement the 3Rs mandate, which, inevitably, increased the cost of insurance rather than decreasing it.
Risk reporting mandates in the US Affordable Care Act created new categories of automated processes and reports under the rubric of “Risk Adjustment, Reinsurance, and Risk Corridors” (3Rs) with the intent of offsetting the impact of rules that protect patients by prohibiting insurers from charging higher premiums or refusing coverage based on preexisting conditions. The motivation was well-intended, but the impact (law of unintended consequences) was opposite of the underlying intent. It cost insurers tens of billions of dollars to implement the 3Rs mandate, which, inevitably, increased the cost of insurance rather than decreasing it.
Furthermore, the specific provisions have stimulated new behaviors in insurers and, by extension, the medical professionals that receive money from them, that may not be in the best interest of patients. These behaviors make patients appear to be at higher risk based on the definitions in the legislation, thus qualifying the insurers for subsidies instead of penalties. I think the “Patient Protection” clauses of the act are great and had positive impacts. But from a holistic perspective, the outcomes have been opposite of the goals of affordability (thus the new euphemism “premium stabilization”). So we have a counterpoint in which computers, instead of improving outcomes and reducing costs, have had the opposite effects.
It should be clear to readers how I feel about the benefits of well-designed automation and the detriments of naïve bureaucracy. Not all automation is well-designed, and not all bureaucracy is naïve. We are all left to let common sense prevail, avoiding knee-jerk reactions, and making decisions (or laws) based on reason rather than fear. Don’t be shy about trusting your diagnosis to a machine, and don’t be shy about confirming it with a qualified medical professional.
| Click below to look in each Understanding Context section |
|---|








